What is the difference between Dementia & Alzheimer’s Disease?
Dementia is an umbrella term used to describe symptoms that result in a decline to cognitive ability, severe enough to interfere with daily life. It is not a normal part of aging. Symptoms of dementia are caused by a number of different disease processes within the brain, of which Alzheimer’s disease is the most common. To summarize, Alzheimer’s disease causes the symptoms of dementia.
What are the early signs and symptoms of dementia?
- Memory loss that affects daily life
- Difficulty performing familiar tasks
- Problems with language
- Disorientation in time and space
- Impaired judgment
- Problems with abstract thinking
- Misplacing things
- Changes to mood and behaviour
- Changes in personality
- Loss of initiative
For more information click here: https://alzheimer.ca/en/about-dementia/do-i-have-dementia/10-warning-signs-dementia
What are the stages of dementia?
The GEMS: Brain Change Model developed by Teepa Snow is the best model I have found to explain what to expect at each stage of dementia. It helps us to understand how things may progress, but also highlights what strengths remain so we can tap into these to foster positive interactions throughout the care continuum.
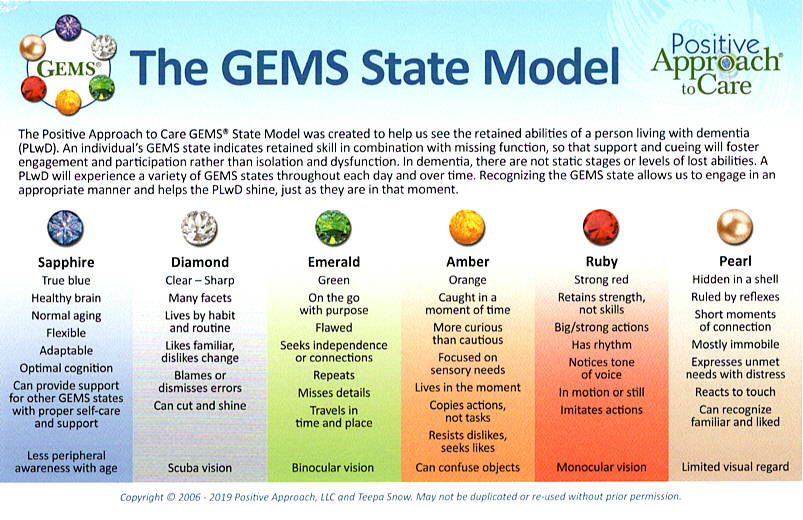
Find out more at https://teepasnow.com/about/about-teepa-snow/the-gems-brain-change-model/
Is dementia hereditary? Does it run in families?
Many people affected by dementia are concerned they may inherit or pass on the condition. One form of Dementia (Familial Alzheimer’s Disease) is passed from generation to generation through a mutated gene. This is extremely rare (less than 1% of cases) and typically impacts people earlier in life with symptoms beginning as early as aged 30-40 years.
Beyond this, there are other variants in genes that can increase our risk of developing Dementia in later life. One example of this is the APOE-4 gene. Having the APOE-4 gene does not cause dementia directly, but it may increase the risk of developing the condition over time. Modifiable lifestyle and environmental risk factors can be adjusted to help us reduce this risk over time.
Is there a cure for dementia?
There is currently no cure for dementia. Due to the variety of factors influencing the development and presentation of dementia, it is unlikely that there will ever be a single cure for dementia.
Research is currently being targeted on finding cures for dementia-causing disease processes such as Alzheimer’s Disease. There are some medications and non-pharmacological interventions that aid in treatment of Behavioural and Psychological Symptoms of Dementia (BPSD).
Are there drug treatments for dementia?
The role of medications in dementia treatments remains limited. in The US Food and Drug Administration (FDA) have approved several medications that fall into 2 main treatment categories:
- Drugs that may change disease progression
- Donepezil (Aricept)
- Rivastigmine (Exelon)
- Galantamine (Razadyne)
- Memantine (Namenda)
- Drugs that may mitigate symptoms of dementia
- Anti-psychotic medications
- Anti-depressants
- Anti-anxiety medications
- Analgesics
- Sleep aids
Please consult your family doctor or memory care specialist to see if drug interventions are recommended for you. It is important that your health provider is made aware of all prescription, and over the counter medications that are currently being taken to determine if there are any associated risks, or contraindications. Any drug interventions should be closely monitored by your medical provider in case of negative side effects.
Medications are often also used to help effectively manage pre-existing health conditions, pain and mood disturbances that could be exacerbating or escalating symptoms of Dementia. Consult your family doctor to find out more.
Alzheimer’s Association (2022) https://www.alz.org/alzheimers-dementia/treatments/medications-for-memory
Are there alternative therapies that may help?
Recent research shows that participation in non-pharmacological therapies can be just as beneficial as any drug treatment in optimizing independence, mood and quality of life of those living with dementia, but without the potential for serious negative side effects.
Alternative treatments include:
- Cognitive Stimulation Therapy Programming
- Music Therapy
- Art Therapy
- Drama & Dance Therapy
- Exercise Programs
- Massage
- Animal assisted therapies
- Sensory stimulation
- Reminiscence Therapy
- Life History work
Is there a way to reduce my risk of developing dementia in later life?
Recent research suggests that there are 12 modifiable risk factors that may reduce our risk by up to 40% of developing dementia in later life.
These are:
- Physical inactivity
- Smoking
- Excessive alcohol consumption
- Air Pollution
- Head Injury
- Infrequent Social Contact
- Less Education
- Obesity
- Hypertension
- Diabetes
- Depression
- Hearing Impairment
I am worried about my memory, what should I do?
If you are noticing changes to your memory you should see your family doctor who can complete an assessment and recommend next steps. Sometimes they will recommend a referral to a local memory care specialist for more in-depth testing. A comprehensive medical assessment will help to rule out any other potential causes of changes to memory or functioning. This usually involves a medical history, physical examination, lab tests such as bloodwork/urinalysis and sometimes a CT or MRI scan of the brain. Additionally, most providers will complete a simple screen of cognition called the Montreal Cognitive Assessment that will help to flag potential areas of concern.
Once this process is completed a diagnosis of dementia can be made. Ask your doctor what type of dementia is suspected, what medication treatments are available and what steps should be taken to get the community based support you need to maintain your independence, well-being and quality of life over time.
How many people in Bermuda have Dementia?
It is estimated that there are currently more than 3000 Bermudians living with a diagnosis of dementia. This number is set to increase along with the aging population.
Globally, Dementia is the fastest growing health crisis, with numbers set to increase along with the aging population, to approximately 139 million worldwide in 2050 (Alzheimers Disease International, 2022 ).
The most recent report from Bermuda’s Department of Statistics (2018) states that seniors aged 65+ will account for 24.9% of Bermuda’s population by 2026. 1 in 10 seniors aged 65+, and 1 in 3 seniors aged 85+ will be diagnosed with Dementia (Government of Bermuda. Department of Statistics (2018). Bermuda’s population projections 2016-2026).
Check out https://www.alzint.org/about/dementia-facts-figures/dementia-statistics/
and https://www.gov.bm/sites/default/files/Bermuda-Population-Projections-2016-2026.pdf for more in-depth information.
Is my loved one still safe to live alone?
Dementia is a progressive condition, which means that we expect things to change over time. Most people will need assistance with daily activities of living as the condition worsens. An occupational therapist can conduct an assessment within the home environment to help you determine the current level of care required, highlight any potential risks or caregiving challenges and put interventions in place to optimize client independence, safety and quality of life over time. They will often provide recommendations relating to compensatory strategies, engagement in meaningful activities, and adaptive equipment aids or home modifications that may be helpful.
It is important to plan ahead if you feel that admission to an assisted living or long term care facility may be required in future. Beds are limited and costs are prohibitive so it is important to plan ahead to avoid crisis scenarios from developing that result in unnecessary acute care or hospital admission in future.
How do I find a caregiver?
Finding a caregiver that is trained, experienced and can develop a therapeutic rapport with the person living with Dementia is key for success. There are a number of private caregivers and agencies available on island.
A list of registered home care providers can be found on https://helpingservices.bm/homecare-providers/
What do I need to do to plan for my future?
Early Dementia diagnosis enables us to access the care and support services we need, when we need them. It also helps us to plan ahead and retain control over our health care decisions as the condition progresses.
Important Steps:
- It is important that you make your future wishes known to your family and friends, and that this information is documented.
- Contact your lawyer regarding issues relating to wills, estates and assigning Enduring Power of Attorney to someone you trust who can make decisions on your behalf in the event that you are no longer able to.
- Contact your banking institution to learn more about how to protect your financial investments, and maintain safe access to daily living expenses when you need them.
- Contact your health insurer to find out what services they offer to support you to remain living within your own home environment for as long as possible. Some insurers will offer in-home care benefits and support access to non-pharmacological therapies that promote optimal health, well-being and quality of life throughout the care continuum.
Final Steps has some fabulous resources to help guide these conversations: finalsteps.bm
Your Conversation Starter Guide: How to talk about what matters to you and have a say in your health care
https://theconversationproject.org/wp-content/uploads/2020/12/ConversationStarterGuide.pdf https://theconversationproject.org/wp-content/uploads/2020/12/DementiaGuide.pdf
My loved one’s condition is progressing rapidly, what can I do?
Dementia is experienced differently by each individual. Each person will move through the stages of the condition at varying rates, and it is common for there to be fluctuations in levels of functional ability. On average persons with a diagnosis of Dementia will have a life expectancy of 5-10 years following diagnosis, however some individuals will live up to 20 years.
Sudden escalations to behaviour and decline to daily functioning are unusual and a red flag for underlying health issues such as infection, pain or delirium. Consult your doctor who will complete a thorough medical assessment and help you determine necessary next steps.
Why is engagement so important for persons living with Dementia?
Engagement in meaningful purposeful activity is a basic human need, and this need does not change with a diagnosis of dementia. Activity participation helps us to feel good about ourselves, interact with others, engage in leisure and social based activities that bring us joy and connection, and enable us to contribute to a community setting.
Engagement to some degree is possible at every stage of dementia. An Occupational Therapist can guide you on how to grade and adapt tasks to optimise your loved ones level of engagement throughout the continuum of care.
Depression and Dementia? Are they related?
Depression is a risk factor for developing dementia in later life. The two conditions are closely correlated with approximately 80% of individuals with a diagnosis of dementia also experiencing symptoms of depression. Depression can also have a significant impact on cognition, mood and daily functioning. Treatment options are available to help. Consult your family doctor or mental health specialist to find out more.
My loved one refuses to go to the doctor, what can I do?
Resistance to seeking medical care and support is common. Your loved one may not be aware of the challenges they are experiencing due to decreased insight. More commonly the early signs and symptoms of dementia have left them confused and scared about what might be happening to them.
It is important to approach them from a place of care and concern. Offer to make the appointment and accompany them to see their doctor to discuss their concerns. Medical assessment will help to rule out any other potential causes of signs and symptoms, and also ensure access to timely treatment and support services if a diagnosis of dementia is made.
Remember we all process information differently, and we are unable to force someone to be receptive to help or support if they are not ready. It may be necessary to repeat the conversation several times before your loved one is more willing to engage in assessment and future care planning.
What strategies can we use to communicate effectively with someone living with Dementia?
Early signs of dementia may include word-finding issues and other communication difficulties. Often this can progress to more marked difficulties with verbal expression, and comprehension. This is termed Expressive and Receptive Aphasia. A Speech & Language Pathologist can assess and provide strategies on how to cope with these changes.
The following general tips can help to foster more effective communication with persons with dementia:
- Minimize other distractions
- Approach from the front
- Speak slowly and clearly
- Maintain eye contact
- Use short, simple sentences
- Keep your tone of voice calm and friendly
- Give the individual plenty of time to respond
- Always include the individual in discussions
- Avoid asking too many questions
- Simplify decisions the individual needs to make i.e. ‘would you like tea or coffee?’
- Use humour to help overcome misunderstandings
- Do not try to correct or argue with the individual. Try to redirect or change the subject instead.
- Use physical contact such as holding the individual’s hand or putting your arm around them to demonstrate affection. Watch the individual’s body language to ensure they are comfortable with this.
Should my loved one be admitted to hospital to get the care they need?
Lack of community based dementia care support services in Bermuda have led to an increase in care crisis scenarios, including caregiver burnout, unnecessary emergency room visits and hospitalization, premature long term care placement and senior abuse and neglect cases. When crisis occurs families often feel that their loved one’s care needs would be best met in hospital.
Unless there is an acute medical issue that requires medical intervention, people living with dementia generally do much better within their familiar home environment. Admission to hospital can be disorienting and anxiety-inducing leading to an escalation of behaviours and use of chemical and physical restraints.
If you have medical concerns, contact your doctor’s office to see if they offer home visits. If hospital admission is necessary ask if a friend or family member can remain with the person with dementia to help reassure and meet their care needs while they receive in-patient care services.
What is Person-Centered Care?
The principles of person‑centred care underpin good practice in dementia care, and assert:
- the human value of people living with dementia (regardless of age or cognitive impairment) and their families and carers
- the individuality of people living with dementia, and how their personality and life experiences influence their response to dementia
- the importance of the person’s perspective
- the importance of relationships and interactions with others to the person living with dementia, and their potential for promoting wellbeing
Anyone caring for a person living with Dementia should have a good understanding of their personal history; including details about their family, life experiences, work history, daily routine, likes and dislikes. This information will help to foster positive interactions throughout the progression of the condition, and also to avoid potential triggers of Behavioural and Psychological Symptoms of Dementia (BPSD) from developing.
Dementia UK offers more information regarding the use of ‘Life History Work” with those living with Dementia https://www.dementiauk.org/life-story-work/
What are BPSD? And how best can we manage them?
Behavioural and Psychological Symptoms of Dementia (BPSD)
Progressing dementia can result in behaviours and changes to personality that are unusual for the person you are caring for. These can be particularly challenging for family and friends who will often compare the current situation with the “way things were”. It is important that we acknowledge that these behaviours are occurring as a result of pathological changes within the brain and are not being done purposely. Try not to take things personally and get the help and support you need to provide the best possible care for yourself and your loved one with dementia.
Drug treatments may not always be the answer. Some behaviours cannot be fixed using medications, and may cause negative side effects that actually make the situation worse.
Instead, consider:
- Pursuing a Comprehensive Dementia Assessment to identify occupational performance issues and assist with problem solving around caregiving challenges
- View behaviour as a method of communication
- Try to identify any potential triggers for behaviours
- It is impossible to remove risk entirely, when we intervene we have to consider what our goals are i.e. keeping someone “safe” from falling by restricting their movements, may actually result in increased agitation, aggression, resistance, depression, withdrawal, immobility, incontinence and skin breakdown.
- Create a structured daily routine that is familiar and predictable for the person living with Dementia
- Be aware of your mindset- your loved one has no control over the progression of their condition. They may be confused, scared and grieving the loss of their independence. Try to put yourself in their shoes and treat them with kindness, love and respect.
- Try to be calm and patient- individuals with dementia will often mirror our communication, behaviour and body language. We must make sure that we are fostering positive interactions and not inadvertently contributing to escalations of behaviour.
- Access caregiver support- caring for someone with Dementia is not a one person job. Taking time for yourself and having the opportunity to voice your challenges and concerns will help you to better care for your loved one over a longer period of time.
Aren’t changes to memory just a normal part of aging?
It is normal for there to be some cognitive changes noted as we age. Our memory may not be as good as it used to be, we may lose track of things, and take more time to process information. However, normal age related changes should not significantly impact our independence and daily functioning. Symptoms of dementia are not a normal part of ageing, and occur as a result of pathological changes within the brain. Symptoms will impact more than just memory, and will result in progressive cognitive and functional decline over time. If you are noticing changes to your memory please contact your family doctor for further assessment. There are other conditions that mimic early signs and symptoms of dementia such as infection, vitamin deficiency and sensory loss. Early assessment and intervention is key to maintaining optimal independence, safety and quality of life while living with a diagnosis of dementia.
Learn more about the difference between normal ageing vs. dementia here: https://www.alzheimers.org.uk/about-dementia/symptoms-and-diagnosis/how-dementia-progresses/normal-ageing-vs-dementia